Thrombotic Thrombocytopenic Purpura (TTP) is a rare and life-threatening hematologic disorder. If untreated, its mortality is as high as 90%. In this article we highlight the most important concepts about the TTP.
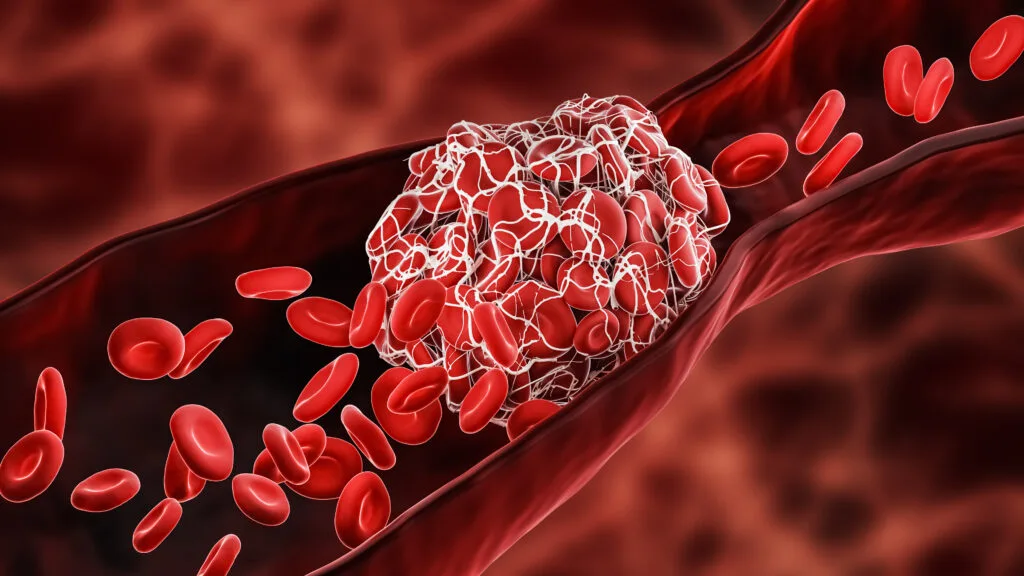
TTP is characterized by microangiopathic hemolytic anemia, thrombocytopenia, and brain and kidney ischemia due to microvascular thrombosis.
Pathophysiology of TTP
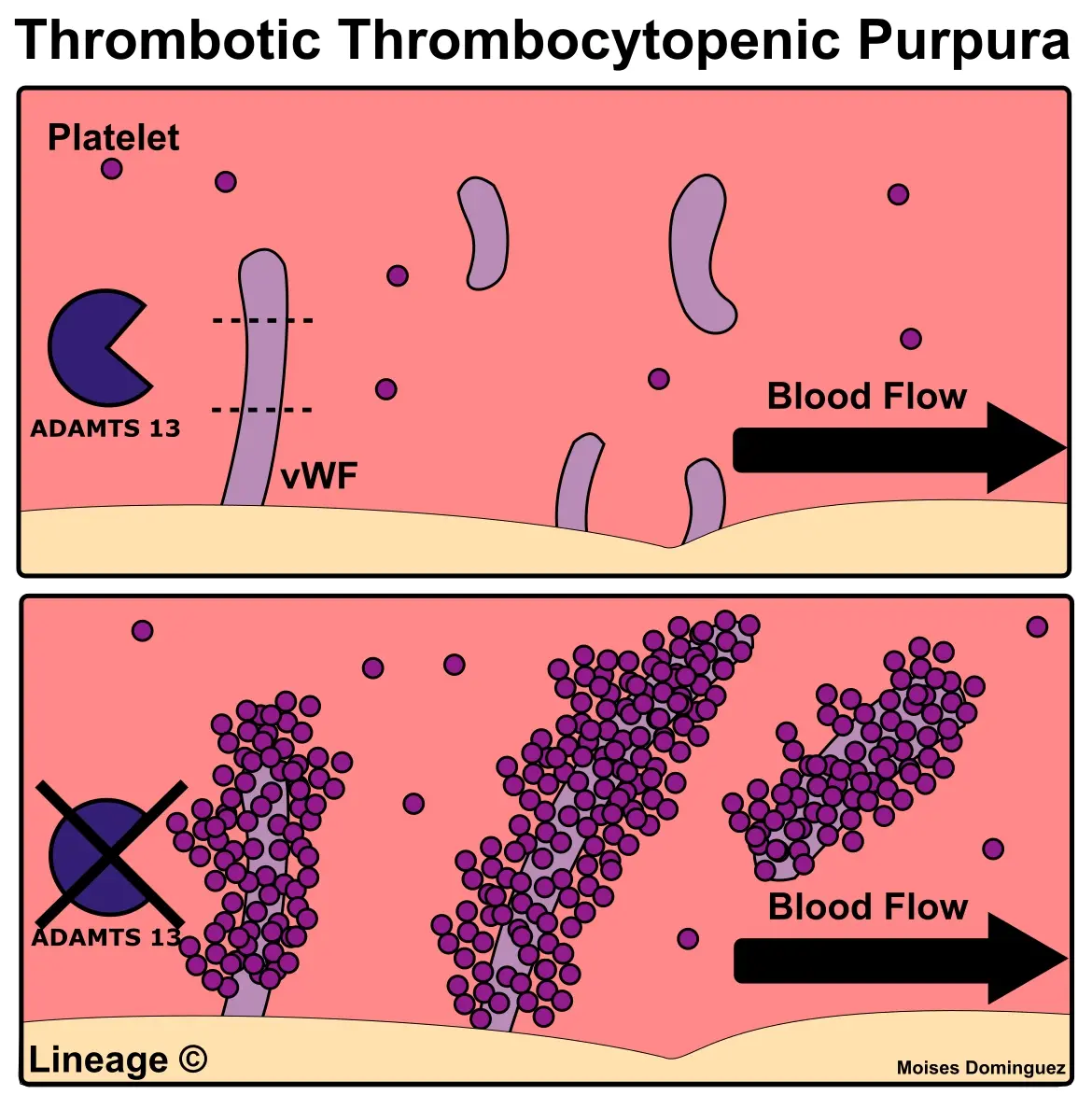
The pathophysiology of thrombotic thrombocytopenic purpura primarily involves a deficiency (congenital) or inhibition (acquired) of the ADAMTS13 enzyme, which is responsible for cleaving von Willebrand factor (vWF) multimers in the lumen of the capillaries. vVF is thrombogenic and causes platelet activation and aggregation. When ADAMTS13 activity is reduced, unusually large vWF multimers accumulate, leading to excessive platelet aggregation and the formation of microthrombi. These microthrombi cause ischemic damage to vital organs, such as the brain and kidneys, leading to the clinical manifestations of the disease.
In acquired form, autoantibodies inhibit the activity of ADAMTS-13. Common triggers for the formation of these autoantibodies include antiplatelet drugs, immunosuppressive agents, HIV, estrogen-containing birth control, and pregnancy.
In TTP, patients suffer from thrombocytopenia due to consumption, meaning that in-lumen thrombosis causes usage of the thrombocytes and therefore thrombocytopenia. Thrombocytopenia exposes patients to the higher risk of bleeding. Most common manifestation of this is purpura, bleeding in the skin.
Diagnosis
Diagnosing involves a combination of clinical evaluation and laboratory tests. Clinically, patients often present with the classic pentad of symptoms: microangiopathic hemolytic anemia, thrombocytopenia, renal dysfunction, neurological symptoms, and fever. However, not all patients exhibit the full pentad. Laboratory findings typically show signs of hemolysis, including elevated lactate dehydrogenase (LDH), indirect (unconjugated) hyperbilirubinemia, and reduced haptoglobin levels.
Schistocytes, fragmented red blood cells, can be seen on the peripheral blood smear. They occur in TTP due to the fragmentation of red blood cells as they pass through small blood vessels obstructed by microthrombi, leading to mechanical damage and shearing.
Confirming the diagnosis often involves measuring ADAMTS13 activity levels, which are usually markedly reduced in TTP (less than 10%), along with the presence of ADAMTS13 inhibitors.
Clinical Presentation
The clinical presentation of TTP can vary, but common symptoms include fatigue, pallor, petechiae or purpura due to thrombocytopenia, and neurological signs such as confusion, headaches, seizures, or focal deficits. Renal involvement may manifest as elevated creatinine levels and hematuria. Fever may also be present, though it is less common. Because TTP can mimic other conditions, such as hemolytic uremic syndrome (HUS), prompt recognition and differentiation are critical for effective management. The acute onset of symptoms, adult age, no recent medical history of gastrointestinal infections, along with laboratory evidence of hemolysis and thrombocytopenia, should raise suspicion for TTP.
MNEMO
P – Purpura (thrombocytopenia)
A – Anemia (hemolytic)
N – Neurological symptoms
I – Increased temperature
K – Kidney (Renal Failure)
Treatment
The cornerstone of TTP treatment is urgent plasma exchange therapy – plasmapheresis. This process removes circulating vWF multimers and ADAMTS13 inhibitors while replenishing functional ADAMTS13. This therapy should be initiated as soon as the diagnosis is suspected, as delays can lead to significant morbidity and mortality. Corticosteroids, such as prednisone, should be administered to reduce inflammation and inhibit the production of ADAMTS13 inhibitors. In refractory cases or relapses, additional treatments like rituximab, an anti-CD20 monoclonal antibody, may be used.
Clinical “Pearls”
Pentad Awareness
While the classic pentad of TTP is helpful for diagnosis, remember that not all patients will present with all five symptoms. High clinical suspicion and early intervention are key.
Schistocytes on Smear
The presence of schistocytes on a peripheral blood smear is an important diagnostic clue and should prompt consideration of TTP in the differential diagnosis of hemolytic anemia.
Urgency of Plasma Exchange
Rapid initiation of plasma exchange can be life-saving. Delays in treatment can lead to irreversible organ damage or death.
Distinguishing from HUS
TTP and HUS share similar features but have distinct pathophysiologies. HUS is more common in children and often follows an infectious gastroenteritis, whereas TTP typically affects adults and has a more pronounced neurological component.
ADAMTS13 Testing
Although ADAMTS13 assays confirm the diagnosis, treatment should not be delayed while waiting for results. Clinical judgment is crucial in initiating therapy.
Conclusion
Thrombotic Thrombocytopenic Purpura (TTP) is a rare and life-threatening disease characterized by extensive microvascular thrombosis leading to multiple organ ischemia. It primarily results from a deficiency or inhibition of the ADAMTS13 enzyme, which is necessary for regulating blood clotting. Diagnosis combines clinical assessment with specific laboratory markers, including reduced ADAMTS13 activity. Prompt treatment with plasmapheresis and corticosteroids is essential to remove abnormal clotting factors and prevent irreversible complications. If untreated, TTP has mortality of 90%. This fact best highlights the importance of fast recognition and management.
Apply Your Knowledge: TTP Case Study
Let’s put your skills to the test with this clinical case. The following 7 questions refer to the same case. Use this scenario to sharpen your diagnostic abilities and decision-making skills, helping you gear up for exams like the USMLE Step 2. Examine the patient’s symptoms, weigh your treatment options, and plan your strategy.
Study with MedBrane
If you’re keen to deepen your understanding of internal medicine, give the MedBrane app a try. It’s free and offers a great way to gauge what you already know through thorough exam simulations. Plus, you can learn as you go with in-depth explanations for every question.
Also you can follow us on Instagram @medbrane for more material for medical students and study tips!